Aug 22 • Sean Overin
Is Pain Just a Psychiatric Symptom? 🤔
Empty space, drag to resize
Hi everyone,
This week’s read is a heavyweight umbrella review by Friedrich et al. (2024) on chronic pain across 13 psychiatric diagnoses. 20 top-tier studies (systematic reviews, large cohorts, RCTs) across ~810k people with mental disorders and ~16.5M controls.
The key point: psychosocial interventions for mental health do improve quality of life and pain interference, but don't expect big shifts in pain intensity. That gap is where we, as physios and rehab providers, play a critical role.
Let's get deeper into this paper.

For me, this review makes it clear that chronic pain prevalence is high, but uneven:
🔄 Importantly, pain and mood feed each other—a bidirectional loop where pain worsens mood, mood amplifies pain, and together they drive disability.
😴 And as we’ve discussed before, Sleep also plays into this cycle: poor sleep heightens both pain and mood symptoms, while pain and low mood disrupt sleep (not covered in this paper, but often part of the picture).
- 🟣 PTSD → ~91% report chronic pain
- 🔵 Depression → ~60%
- 🟢 Bipolar disorder → ~60%
- 🟠 Schizophrenia → ~30% (often under-recognized)
- 🟡 ADHD/ASD → high multisite pain, especially in females
🔄 Importantly, pain and mood feed each other—a bidirectional loop where pain worsens mood, mood amplifies pain, and together they drive disability.
😴 And as we’ve discussed before, Sleep also plays into this cycle: poor sleep heightens both pain and mood symptoms, while pain and low mood disrupt sleep (not covered in this paper, but often part of the picture).
What else to know...
🧠 Psychosocial interventions are well studied: CBT, mindfulness-based cognitive therapy, and polypharmacy approaches reliably improve mood and functioning. But the effect is selective:
⚠️ Diagnostic overshadowing is real. In psychosis, pain often gets dismissed or missed. Careful assessment matters.
🧘 Body-based practices (yoga, tai chi, etc.) → stronger effects on pain than purely psychosocial treatments.
- 👍 Pain interference & self-efficacy improve → people do more, feel more capable
- 👎 Pain intensity? Largely unchanged. That needle rarely moves.
⚠️ Diagnostic overshadowing is real. In psychosis, pain often gets dismissed or missed. Careful assessment matters.
🧘 Body-based practices (yoga, tai chi, etc.) → stronger effects on pain than purely psychosocial treatments.
For Movement-based Rehab Providers
👉 The signal is that interference matters most. Pain scores may barely budge with psychosocial interventions, but interference drops in meaningful ways—patients are doing more despite similar pain intensity. That's obviously important.
A few other practical insights stood out:
A few other practical insights stood out:
- 🔎 Diagnostic overshadowing → don’t rely on self-report alone. Use functional tests and document interference to capture impact.
- 💡 Treatment signals → CBT helps, but movement & body-based practices (yoga, tai chi, exercise) often reduce pain more when mental health conditions co-occur.
- 🏋️ First-line role → movement-based interventions shift pain, mood, and sleep together
- 💊 Opioid exposure → people with serious mental illness are disproportionately prescribed opioids. Physios and other movement-based rehab providers can offer non-opioid alternatives—graded activity, pacing, sleep strategies, and collaboration with mental health providers.

The big insight: again, psychosocial interventions alone aren’t enough to reduce pain intensity. They improve coping and role participation, which are essential—but rehab providers must keep advocating for the physical side of the equation. And equally, our psychiatric and mental health colleagues should loop physios and other rehab providers in as partners so patients receive both sides of care: mental health support and body-based strategies for pain.
What else should we consider…
🎯 Dual targeting → combine psychosocial and physical rehab.
📊 Track interference, but aim for intensity too → interference and self-efficacy are our north stars, but patients still care about intensity.
🏋️ Make your lane clear → education, graded activity, specific exercise, manual therapy, and physical health approaches remain under-advocated.
🤝 Collaborate → build trusted mental health partnerships and make your value visible as a movement-based provider.
🔎 Recognition → pain is a distinct, treatable condition—not just a psychiatric symptom.
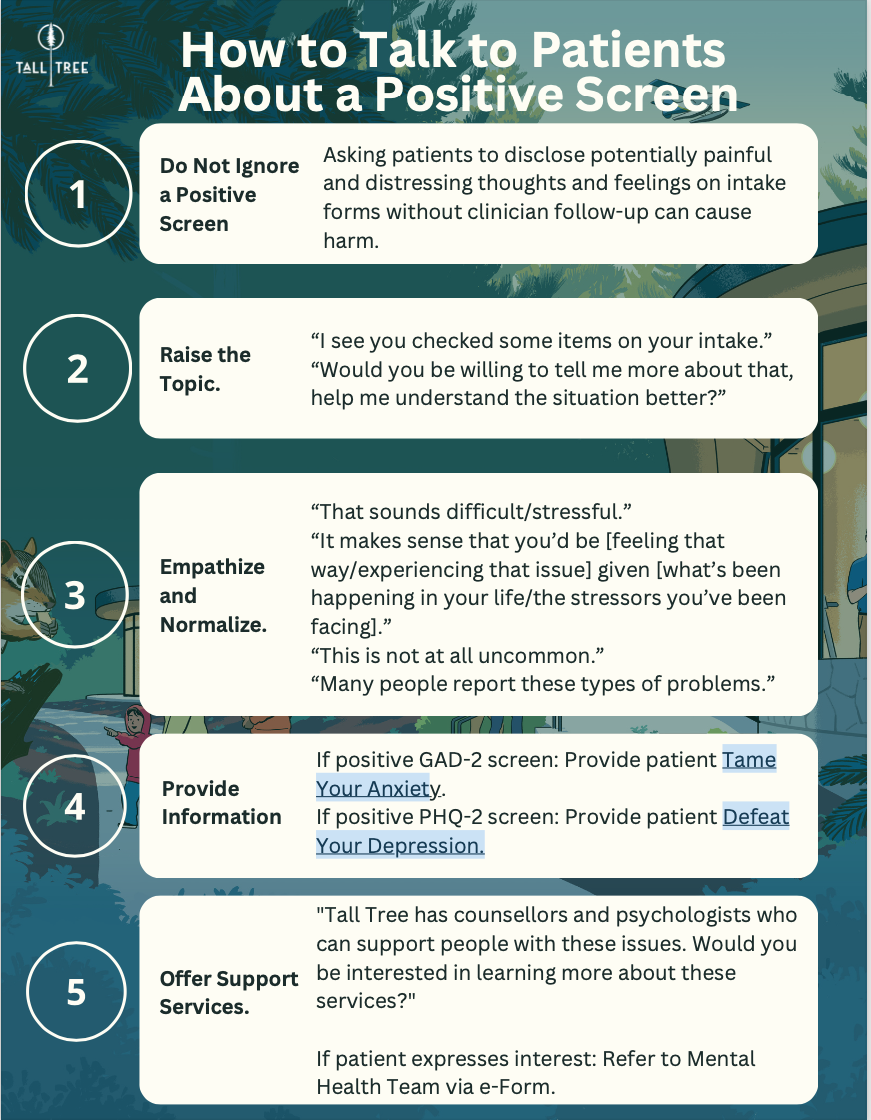
🧾 Screening → PHQ-2 / GAD-2 (≥3/6 = I pause for a short chat and, if needed, connect them with resources or referral)
🌐 Build your referral network → know your local and virtual providers so referrals are smooth and confident. Don't have one, send them here.

Aim: Pick up more comorbidity and demonstrate interference gains.
Week 1 (with any patient with chronic pain +/- MH Dx):
Week 1 (with any patient with chronic pain +/- MH Dx):
- Add one screening line: “Over the past week, how much did pain interfere with your general activity (0–10)?”
- If you suspect depression or anxiety, run a quick PHQ-2/GAD-2. If ≥3, have a short, supportive conversation and connect them with resources or referral.
- Re-measure interference and one function test.
- Share the progress back to the patient. (“You went from 6/10 interference to 4/10, and added two more sit-to-stands.”) That feedback loop builds buy-in.

Course for Clinicians: Addressing Mental Health Concerns in MSK Populations
Live trauma-informed care training: Practical Trauma‑Informed Care for Health Care Providers
- The course I wish I had early in my career...A short, practical, course on why screening matters, how to use PHQ-2 and GAD-2, how to have these first conversations, and how to build referral pathways (including if you don’t have a trusted local network).
- This is one step towards psychologically-informed care.
Live trauma-informed care training: Practical Trauma‑Informed Care for Health Care Providers
- A four-session, live-online course (8 hours total) starting in October 2025, led by OT and mindfulness teacher Cassi Starc.
- You’ll walk away with tangible tools to:
- Recognize trauma signs confidently,
- Create safety in your sessions,
- Respond compassionately in the moment, and
- Build a self-care plan to sustain your own wellbeing.

Make pain interference one of your North Stars, but not the only one.
With psychosocial interventions, we probably shouldn’t expect pain intensity to move much. Patients often expect otherwise—and when pain scores don’t change, frustration can creep in, sometimes leading to the conclusion that “this pain is just in my head.” Maybe the narrative is different for pain reprocessing therapy, but we need more evidence first.
Importantly, this paper isn’t a critique of mental health professionals—they’re doing hard, necessary work. Instead, it’s about seeing the bigger picture. The evidence consistently points to three levers:
🧠 Cognitive approaches (CBT, mindfulness, acceptance-based care)
💊 Pharmacological approaches
🏃 Movement practices
The real win? Integration.
👉 When patients are guided into good first-line MSK pain care—alongside mental health support—lots can happen. Perhaps they begin doing more, living more, rely less on meds and see reductions in pain intensity too. That’s the dent we can make.
Stay nerdy,
Stay nerdy,
Sean Overin, PT
Subscribe to our newsletter
Every Friday we cover must read studies, how they fit in practice, give it real world context, provide top resources and one sticky idea.
Thank you!
You have successfully joined our Friday 5 Newsletter subscriber list.
