
Chen et al., Pain (2018): A 5-year back pain crystal ball.
Unfortunately, the narrative that “it’ll just get better” doesn’t hold up.
This study followed people for 5 years and found 4 clear pain trajectories—plus some early flags for who’s likely to struggle:
Unfortunately, the narrative that “it’ll just get better” doesn’t hold up.
This study followed people for 5 years and found 4 clear pain trajectories—plus some early flags for who’s likely to struggle:
🔍 The 4 Pain Paths
- No or Occasional Pain – These folks bounce back fast. 🙌
- Persistent Mild Pain – Some nagging, but manageable.
- Fluctuating Pain – Up, down, up again—like a yo-yo 🎢
- Persistent Severe Pain – The tough one. Pain sticks around. 😣
Spoiler: 25% landed in the persistent severe group—but that’s the crew we’re most worried about.
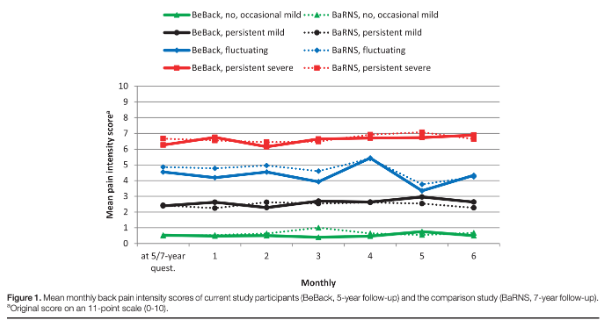
This figure shows the four long-term pain trajectories identified in the Chen et al. (2018) study, comparing two different cohorts: BeBack (5-year follow-up) and BaRNS (7-year follow-up).Each line represents mean monthly back pain intensity scores over time (0–10 scale):
🧠 Key insight: These patterns are remarkably stable over years—reinforcing the idea that early identification of trajectory (and intervening accordingly) could change someone’s long-term experience of back pain.
- Green (No or Occasional Mild Pain): Very low pain throughout—consistently around 0–1.
- Black (Persistent Mild Pain): Steady low-level pain (~2–3), showing little fluctuation.
- Blue (Fluctuating Pain): Pain levels bounce around (4–5), with noticeable month-to-month shifts.
- Red (Persistent Severe Pain): Consistently high pain (~6–7) across the entire follow-up period.
🧠 Key insight: These patterns are remarkably stable over years—reinforcing the idea that early identification of trajectory (and intervening accordingly) could change someone’s long-term experience of back pain.
🚨 Who’s at Risk for a Rough Ride?
Some signs scream “this could get sticky”—and they show up early.
🔬 Early life adversity & genetics – Set the stage for a sensitive system
😰 Chronic stress – Keeps the volume knob turned up
🧠 Mental health conditions – Depression, anxiety, trauma = higher risk
🔥 Higher baseline pain – The fire’s already burning
😟 Unhelpful beliefs – “I’ll never get better,” “My back is damaged”
🛋️ Passive coping – Resting, guarding, avoiding
📉 Lower socioeconomic status – Social disadvantage makes everything harder
👉 Spot these early, and we’ve got a better shot at changing the story.
🧠 Translation: People weren’t doomed by their back—they were thrown off course by fear, beliefs, and life stress. This really aligns with what patients expect from their therapist — a plan that addresses biology and psychology.




