Feb 20 • Sean Overin
Two Alarms, One Outcome: Rethinking Chronic Pain
Empty space, drag to resize
Another heavy-hitter just dropped from the UK Biobank:
“Biological markers and psychosocial factors predict chronic pain.”
It’s a massive study — over 500,000 participants — and yes, the paper is a beast to read. But here’s the cleanest takeaway:
- Biological markers (like CRP, HDL, neutrophils) predict the presence of pain-related diseases (think gout, MS, arthritis).
- Psychosocial markers (sleep, stress, mood, beliefs) predict the experience of pain — how intense it feels, how widespread it is, and how long it sticks around.
- Put them together, and you’ve got a powerful predictor of who’s in trouble now, and who’s heading for long-term, persistent pain.
With this level of data, we can finally move beyond the old “Is it the tissue or is it the mind?” debate.
Spoiler: it’s both.
Empty space, drag to resize
Let’s dig in a little deeper — and explore what this actually means for practice.
Take a breath... here we go.

🔬 What the researchers did (I think)
Using data from over 500,000 people, the researchers looked at two types of pain:
- Diagnosed pain conditions — confirmed medical diagnoses (e.g., gout, MS, osteoarthritis, fibromyalgia).
- Self-reported pain — survey responses on where people hurt, how much, and how widespread. No doctor needed — just the person’s lived experience.
To predict who had pain or was likely to develop it, they collected three types of data:
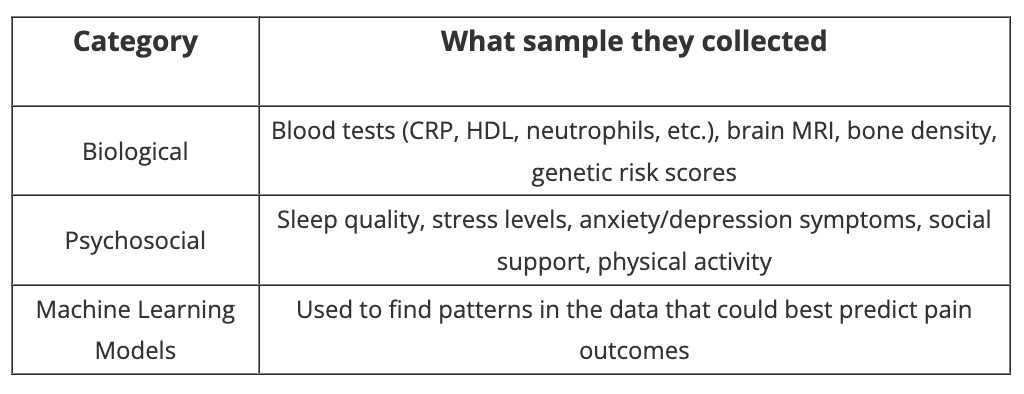
They used these data to answer three big clinical questions:
- Who already has a pain diagnosis?
- Who reports chronic or widespread pain even without a diagnosis?
- Who’s likely to develop chronic pain in the next 5–15 years?
💡 Simple translation:
They ran labs, imaging, and lifestyle surveys to predict:
- What’s happening now
- What people are feeling
- What’s coming next
🔑 Key finding:
- Blood tests predict disease.
- Mood, sleep, and stress predict pain.
- Together, they predict who’s suffering now — and who’s next.
🔍 Go one level deeper:
Biomarkers => predict diagnoses like gout and MS
Psychosocial => pain intensity, spread, and persistence
Both combined =>
- One red flag (bio or psycho) → 6–18× more likely to already have a chronic pain diagnosis
- Two red flags (bio + psycho) → 18–42× more likely
2× the future risk of developing chronic pain over 15 years
Okay, let’s take a moment. And maybe another one.
I told you this paper was a bit of a beast. Thanks for hanging in there...seriously.
Let's try and see what this means for clinical practice.

So what does this potentially mean?
If someone walks into your clinic with pain, we want to at least think about two things:
What’s going on in their body (inflammation, bone health, metabolic health etc.)
What’s going on in their life (sleep, stress, mood, activity levels, etc)
Here’s why
- Biology tells you if this is a disease related pain problem
- Psychosocial factors tell you how much it might hurt, how much it spreads, and how long it might last.
- If both are lit up, they’re in trouble. Again, these patients are:
- Up to 42× more likely if both systems are firing
- Twice as likely to develop chronic pain down the road
Translation:
A blood test without a sleep check might miss the risk.
A mood screen without a CRP might miss the mechanism.
But together, they help you spot the patient who needs more than just exercises and reassurance.
Test broadly. Act early. And never assume pain is just one thing.

To highlight how this might look in practice, let's use a case study:
👩⚕️ Meet Sarah
Sarah is 46. She comes in with ongoing neck and shoulder pain that's been flaring for the past 6 months. Recently, mild pain has started showing up in the upper back.
Her imaging? Totally clean.
Her blood work? Low-grade inflammation (CRP slightly elevated) from her last panel.
But here’s what you notice during your intake:
- She’s sleeping 5 hours a night and self-reports "poor sleep"
- Reports "high" work stress
- Scores positive on the PHQ-2 (4/6)
The Physical Exam looks pretty darn good:
- Neck AROM within normal limits with end of range stiffness reported
- Cervical Flexion Rotation Test WNL
- Shoulder AROM within normal limits with end of range upper back pain noted
- Neurological exam is unremarkable; mild tension in the ULTTA on the right
- Mild tenderness on palpation of the neck and shoulder region
She says:
“I feel like my body’s falling apart, but no one can find anything wrong.”
How this study helps you reframe Sarah’s case:
Instead of chasing more scans or just telling her to move more, you recognize:
- Biology is mildly active (inflammation is whispering)
- Psychology is fully lit (stress, sleep, mood)
According to the UK Biobank findings:
- Sarah already has higher odds (6–18×) of sitting in the chronic-pain category.
- Because both systems (bio + psycho) are red-flagged, she’s in the high-risk group for persistent pain over the next decade — up to 2× the long-term risk.
🎯 What you do differently:
- Validate that her pain is real, even if her scans are clean
- Share the “two-alarm” metaphor (body + brain both shouting)
- You might even differentiate nociceptive versus nociplastic pain.
- Offer simple coaching or ask to offer information to help with sleep and stress
- Flag her for a collaborative plan: physio + psych + possible GP follow-up
💡 Why it matters:
Without this lens, Sarah might bounce between providers for years, chasing answers in her joints.
With it, you’ve reframed her case, offered a roadmap, and changed the story before it calcifies.
That’s the power of biopsychosocial insight — it doesn’t take more time, just a broader lens.

Here is some stuff to help support bringing the 'psycho' into a biopsychosocial model of care:
Mental Health Guides
These four supportive guides offer practical tools to manage anxiety, low mood, and unhelpful thought patterns. Created to support your practice and a patient's mental health journey with insight and care.
Seamless Mental Health Referrals
A practical PDF for healthcare providers to learn how to identify mental health concerns, navigate referrals, and match clients with the right support. Ensure your patients receive timely, effective, and compassionate care.
Free Science-backed Programs
When someone signs up for one of these programs, they receive a curated series of short, evidence-based emails delivered over several weeks. Each message is designed to help people learn, support behaviour change, take control and support recovery with clear, practical guidance. This stuff is grounded in the latest research, shaped by clinical experience and compassionate encouragement.
The most relevant one's for today is of course the Sleep Reset Program and Know Pain, Know Gain.
Sign up here
Sign up here

“Pain lives where tissue meets story.”
You’re not just treating muscles or mood. You’re treating the intersection of both.
Engage in shared decision making.
Test broadly.
Listen deeply.
Adjust both levers.
Empty space, drag to resize
A patient walks in with pain.
If you only test the blood, you might miss the storm.
If you only ask about stress, you might miss the fire.
But if you check both, you catch the risk early and change the outcome.
That’s not soft science. That’s clinical power.
Happy Friday — go check both alarms.
Stay nerdy,
Sean Overin, PT
Subscribe to our newsletter
Every Friday we cover must read studies, how they fit in practice, give it real world context, provide top resources and one sticky idea.
Thank you!
You have successfully joined our Friday 5 Newsletter subscriber list.
