Pain That Won’t Budge? Start by Treating Sleep
It might be sleep.
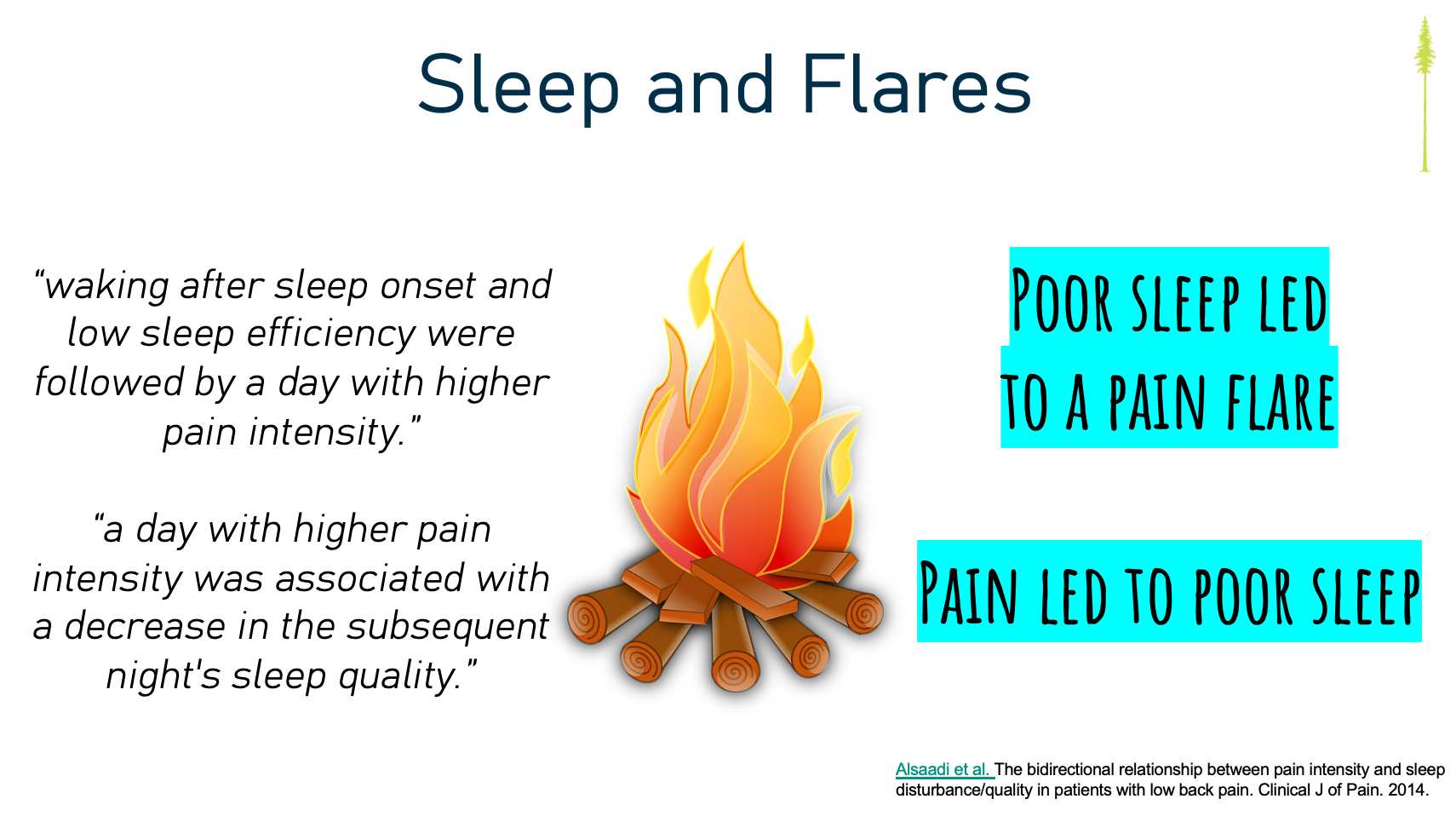
We often hear that pain disrupts sleep — and that’s true. But what’s more surprising (and clinically important) is that sleep problems often precede pain, predict flare-ups, and degrade the body’s built-in pain regulation system. This isn't theoretical. It’s well-studied, repeatable, and should probably change how we prioritize treatment.
Let’s get into it.

Here’s what they found:
- A single night of poor sleep can increase next-day pain intensity
- Sleep disturbance blunts the brain’s descending inhibitory pathways — our natural pain dampeners
- It raises the risk of pain flares and the transition to chronic pain
- People with chronic pain who sleep poorly report more pain, more disability, and more distress
Let that sink in. Sleep disruption isn’t just a symptom — it’s a causal driver of pain sensitivity and chronicity. If your patient isn’t sleeping, you might be treating pain on a tilted table.

Here’s what we might do differently:
- Ask better questions: “Do you fall asleep easily?” “Do you wake up rested?” “Is your sleep pattern predictable?” "Do you have daytime impairment because of sleep?"
- See if there is sleep rides alongside pain flares
- Reposition sleep as a core treatment target, not an optional add-on if were not making progress.
When patients see the link for themselves — “Yeah, I do flare after two bad nights” — they become more open to behaviour change.
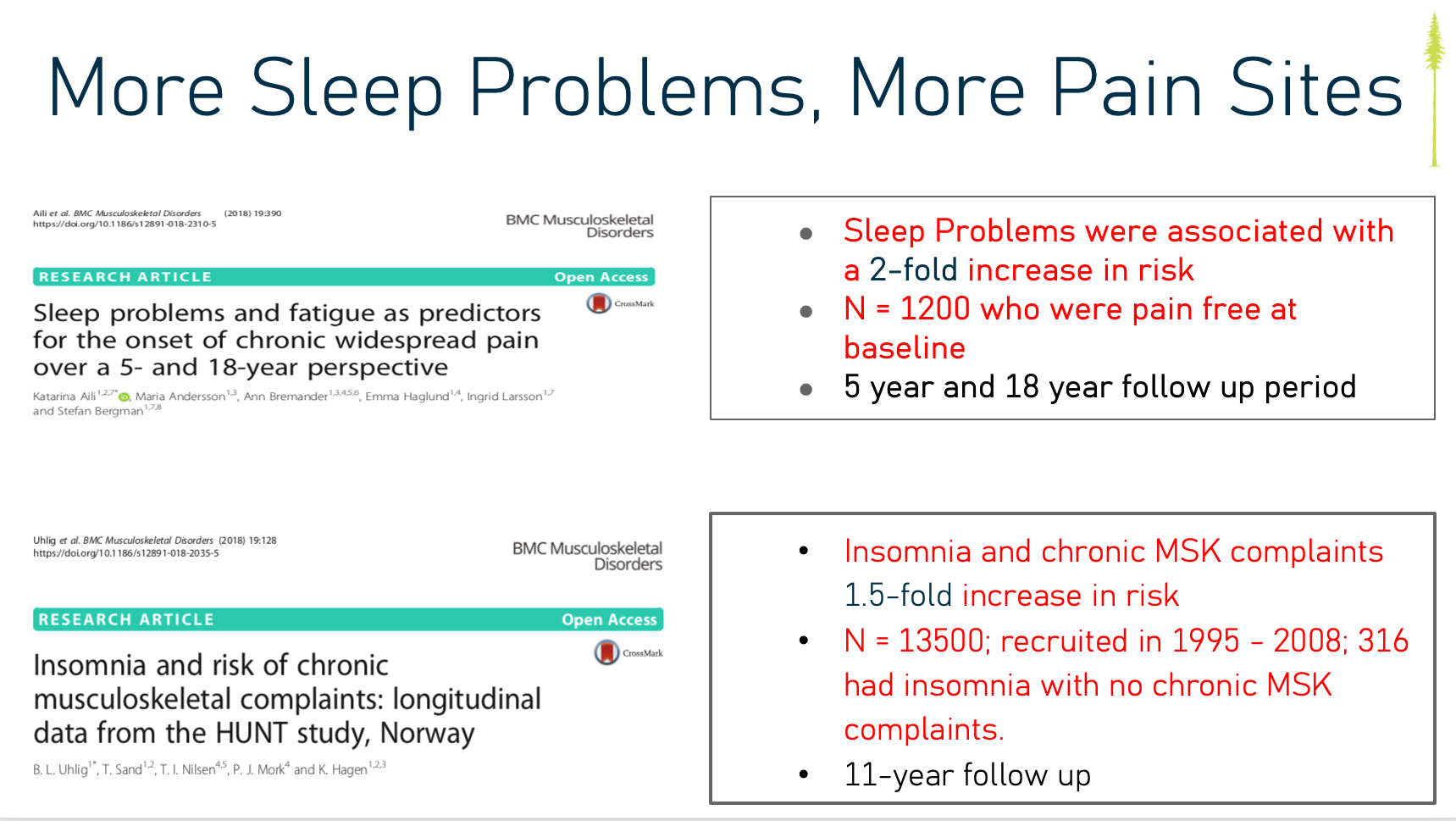
- People with frequent sleep problems were 1.4x more likely to develop chronic pain
- Those with severe insomnia had 2x the risk
- The relationship was dose-dependent — worse sleep = higher pain risk
- And notably, sleep problems predicted pain even in people with no pain at baseline
In other words: chronic pain may begin in the bedroom, not the clinic.
This study is a quiet alarm bell. If we want to reduce the burden of chronic pain, we need to stop waiting for it to show up and start asking about, and treating, sleep disturbance before pain becomes entrenched.
If your patient is stuck in a loop of poor sleep and persistent pain, try this in conversation:
🛠 “Here’s What We Can Do Next…”
“I we think your sleep might be playing a role in your pain experience. We’ve been working hard in rehab, but if your nervous system isn’t doesn't seem to be rested, it’s like trying to recover on a tilted playing field.”
Then offer one of three paths:
- Refer out → “Let’s get you connected with someone trained in CBT-I — Cognitive Behavioral Therapy for Insomnia. It’s the gold standard and it works, even when pain is in the picture.”
- Co-treat → “We can keep working together while sleep is being addressed. You may find things shift more quickly once your system’s less on edge.”
- Pause & reboot → “In some cases, it makes sense to press pause on rehab. Give sleep the attention it needs, then come back stronger — mentally and physically.”
“Better sleep won’t solve every pain problem. But it just might solve the one we’re working on, in part.”

↳ A structured, free, 4-week email campaign to help people build better sleep habits. Rooted in evidence and behavioural science.
📚 Finan et al., 2013
↳ Essential read. If you’ve ever wondered whether sleep is clinically relevant to MSK rehab — this is the paper that answers it.
📚 Skarpsno et al., 2019 — HUNT Study
↳ Hard to ignore: this study makes the case that sleep predicts pain — not just in those already hurting, but in the general population.
📄 Katie Siengsukon, 2018 — Sleep Promotion in Physical Therapy
↳ A primer on how clinicians can screen for sleep dysfunction and incorporate succinct sleep interventions into MSK rehab.
🧠 Coming Soon: CBT-I for Healthcare Pros
We’re about to release a self-paced, online course with Dr. Colleen Carney, one of North America’s leading sleep experts. You’ll learn practical CBT-I tools to integrate into care — no psych degree required. Get on the waitlist and be the first to know when it is released!

“Chronic pain might not start in the tissue — it might start in the nights no one’s asking about."
The HUNT Study reminds us: people don’t just wake up one day with chronic pain. Maybe they build toward it silently, over months and years of restless nights, shallow sleep, and early waking.
By the time that patient limps into the clinic, the problem may not be just what they lifted or how they moved — It may be the hundred nights before that, when their system stopped getting what it needed to recover.
Perhaps that’s the real timeline. And it’s easy to miss if we don’t ask.
Wrapping Up
Sleep is not just a lifestyle factor, it’s another clinical variable. And in some cases, it’s the quiet culprit behind stalled progress, unexplained flares, and patients who just “aren’t getting better.”
Poor sleep isn’t just a side effect of pain. It’s a risk factor. It’s a driver. And it’s another lever to pull. Whether that means co-treating with a CBT-I provider, pausing rehab to focus on rest, or weaving sleep strategies into your care plan, addressing sleep might be the upstream move that unlocks downstream results.
Stay nerdy,
Sean Overin, PT
Subscribe to our newsletter
Every Friday we cover must read studies, how they fit in practice, give it real world context, provide top resources and one sticky idea.
Thank you!
You have successfully joined our Friday 5 Newsletter subscriber list.
